Ongoing management of hypoparathyroidsim
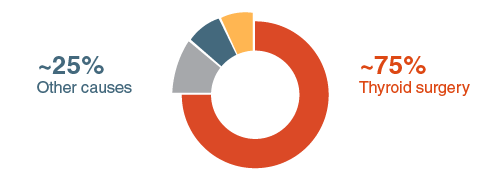
Hypoparthyroidism (hypopara) is a rare disease caused by absent or low levels of parathyroid hormone (PTH) to be secreted from the parathyroid gland.This causes a mineral imbalance in the body including low blood concentration of calcium (hypocalcaemia), high blood concentration of phosphate (hyperphosphatemia), and reduced levels of activated vitamin D, which reduces absorption of calcium in the gut.
Hypopara is often a chronic, life-long rare diesease which requires on-going management. The best management strategies will vary from person to person, and may change over time. Lifestyle changes can often help in the management of symptoms and improving quality of life (QoL) for those with hypopara.
There are a number of different treatment options for hypopara, but the conventional therapy for patients is a regimen of calcium and active vitamin D supplements. Calcium supplementation maintains calcium levels and can treat the symptoms of hypocalcaemia. PTH has the important role of converting vitamin D in the body to an activated form, which can increase the absorption of calcium; therefore the management of hypopara usually consists of a balance between calcium and vitamin D supplements. Though many patients can manage hypopara with conventional therapy alone, some patients find that conventional therapy is not sufficient to manage their hypopara. Complications can also sometimes occur due to hypercalcaemia as a result of long-term treatment with calcium supplements.
Managing hypopara with your diet
Calcium intake from food can be evenly distributed throughout the day, which can reduce the need for high doses of calcium supplementation. Some patients may choose to try to manage their hypopara through dietary changes; by eating calcium-rich food and avoiding meals with high phosphate content, either with or without a supplement regimen. Natural sources of calcium include: dairy, soya, green leafy vegetables, beans and lentils, nuts, fish and foods made with fortified flour. Dietary phosphate can also be reduced by avoiding processed foods. Activated vitamin D supplements can imrove the rate of absorption of dietary calcium in the intestine. Patients should discuss the best management strategy for them with their physician before changing their diet.
Calcium content of some calcium-rich foods based on the average serving size: